Mission:
“Premier Healthcare Compliance is dedicated to providing smarter compliance solutions that help healthcare providers reduce risks, optimize operations, and maintain healthier clinics. We aim to make compliance easier, more effective, and aligned with the highest standards of patient care.”
Vision:
“Our vision is to be the go-to partner for healthcare providers, helping them create sustainable, compliant practices that lead to better care outcomes and organizational success.”
Values:
- Innovation: We constantly evolve to provide smarter, more effective compliance solutions.
- Collaboration: We work closely with healthcare providers to meet their unique compliance needs.
Integrity: We uphold the highest ethical standards in every service we provide.
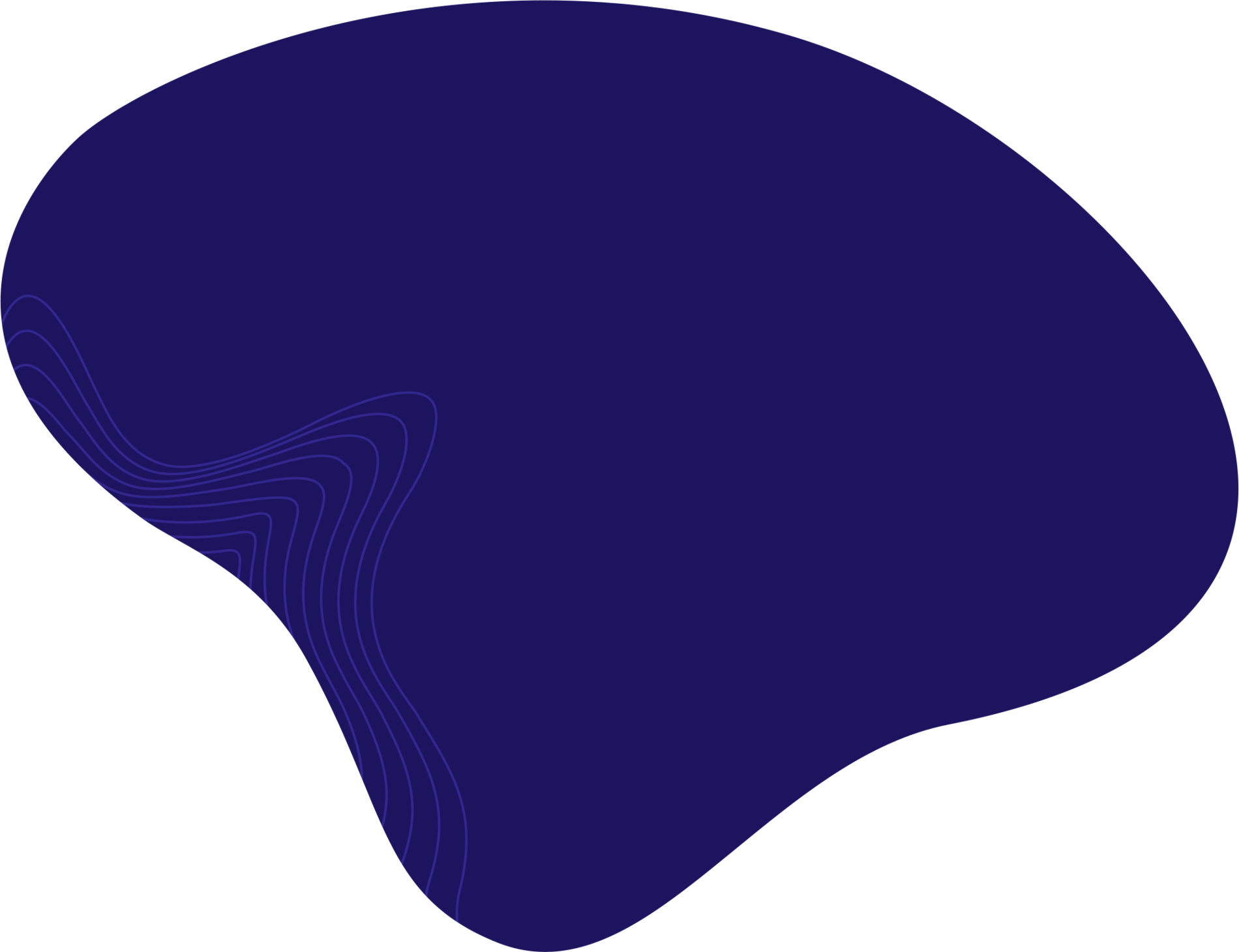
Face Fines Up to
$100,000 for Non-Compliance
with CMS Rules
Failure to follow CMS guidelines, including overpayments, improper billing, and non-adherence to Medicare or Medicaid, can result in penalties of up to $100,000 per violation under the False Claims Act (FCA).
Reference: U.S. Department of Health & Human Services, Office of Inspector General (OIG). False Claims Act Overview.
Abuse (FWA) Prevention
Fraud Prevention
Programs Cut
Healthcare
Losses by 20%
Healthcare fraud costs the U.S. government $60-80 billion annually, but effective Fraud, Waste, and Abuse (FWA) prevention programs can reduce losses by up to 20%.
Reference: National Health Care Anti-Fraud Association (NHCAA). The Challenge of Health Care Fraud.
Non-Compliance
Costs Average
$14.82M
Per Data Breach
Organizations that fail to meet regulatory guidelines, like HIPAA, face an average cost of $14.82 million per breach, including fines and reputational damage.
Reference: National Health Care Anti-Fraud Association (NHCAA). The Challenge of Health Care Fraud.
Compliance Reviews
Reduce Violation
Risk by
Up to 50%
Regular compliance reviews and risk assessments can lower non-compliance risk by 40% and reduce costly violations by 35-50%, helping healthcare organizations meet regulatory standards.
References: U.S. Department of Health & Human Services (OIG); American Health Law Association (AHLA).
With experience in healthcare regulatory issues, including the False Claims Act, Stark Laws, and Anti-Kickback Statute, we ensure that your clinic or hospital is protected from legal risks and remains aligned with industry standards. Our bilingual team facilitates clear communication with diverse healthcare teams ensuring smooth collaboration in regulatory matters.
What sets us apart?
We bring insights from our years of working directly for the health insurance industry, meaning we understand both sides of the equation—payer and provider. This gives us a unique advantage in guiding you through the compliance process with a perspective rooted in experience and precision.
Our Expertise: Why We Make a Difference
Navigating Guidelines
- Medicare Guideline Interpretation: With extensive knowledge of Medicare and its intricate guidelines, we help providers adhere to compliance requirements, ensuring that billing and documentation are accurate and aligned with federal standards.
Fraud, Waste, and Abuse (FWA) Prevention:
Our professionals have years of experience in FWA detection and prevention, collaborating with state and federal law enforcement agencies to protect healthcare organizations from the risks of non-compliance.
Payment Negotiation & Regulatory Expertise:
Our team has negotiated payments and settlements on behalf of health insurance companies, and we have successfully managed high-stakes investigations into complex healthcare fraud cases.
Compliance Reviews & Risk Assessments
We specialize in conducting compliance audits and risk assessments, helping healthcare providers avoid costly penalties associated with regulatory breaches.
Medicare & Medicaid Improper
Payments Hit $86.49 Billion in 2021
In FY 2021, improper payments for Medicare and Medicaid totaled $86.49 billion. Clinics with strong compliance programs can achieve 90% or higher claims accuracy by adhering to CMS guidelines.
Fraud Prevention
Boosts Efficiency by 25%
Organizations committed to regulatory compliance see a 25% rise in operational efficiency, reducing administrative costs and minimizing risk through robust fraud prevention measures.
Locations
Miami
Port St. Lucie
Orlando
Maryland
phones
Phone: +772-333-4414
support
admin@
premierhealthcarecompliance.com
hours
Monday-Friday: 8:00 – 5:00